
Throat Clearing Relief and Treatment
Frequent throat clearing is one of the 4 most common symptoms of Throatburn reflux, along with chronic cough,...
- by Dr. Aviv
- Friday October 10, 2014

Acid Reflux: Heartburn
Heartburn is best described as a burning sensation in the bottom of the chest and ribcage that can expand...
- by Dr. Aviv
- Friday October 10, 2014
Throatburn Reflux
Throatburn reflux is a term that I coined that means acid reflux disease without the classic symptoms of heartburn ...
- by Dr. Aviv
- Saturday November 1, 2014
Chronic cough
Chronic cough, defined as cough lasting for more than 8 weeks, is the most common reason patients see a doctor...
- by Dr. Aviv
- Saturday November 29, 2014
Hoarse voice, raspy voice
Hoarseness is defined as a raspy or strained voice which can be due to many causes....
- by Dr. Aviv
- Saturday November 29, 2014
I have a lump in my throat (globus sensation)
Globus is a Latin word for globe or sphere, which is what people often describe when they come in to see...
- by Dr. Aviv
- Saturday November 29, 2014

Post Nasal Drip (PND)
Post nasal drip (PND) refers to the sensation of mucus or secretions coming down from the back of ...
- by Dr. Aviv
- Saturday November 29, 2014
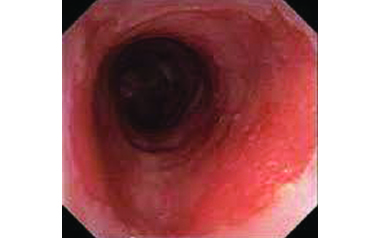
Barrett Esophagus
Barrett esophagus is a potentially pre-cancerous condition typically appearing in the area where the lower part of ...
- by Dr. Aviv
- Saturday November 29, 2014

RISKS OF SEDATION DURING UPPER ENDOSCOPY
There are almost 10 million upper endoscopies performed annually in the USA....
- by Dr. Aviv
- Saturday November 29, 2014

TransNasal Esophagoscopy (TNE)
TNE stands for TransNasal Esophagoscopy. It is a method of examining the esophagus....
- by Dr. Aviv
- Saturday November 29, 2014

SUMMERTIME SMOOTHIE
For a delicious, healthy, replenishing, non-acidic, AcidWatcher-safe smoothie try the Dr. Aviv...
- by Dr. Aviv
- Thursday May 21, 2015

COLORFUL CHICKEN SALAD
Preheat the oven to 450° F. Place the chicken in a pan and sprinkle with olive oil and a pinch of salt. Place the...
- by Dr. Aviv
- Monday July 6, 2015

ALTERNATIVE TO CHIPS & DIP
Roasted Beets and Fresh Cucumber with Creamy White Bean Dip ...
- by Dr. Aviv
- Tuesday July 14, 2015

Acid Watcher® Nicoise Salad
Acid Watcher® Nicoise Salad...
- by Dr. Aviv
- Sunday July 19, 2015

Mexican Shrimp Salad with avocado, black beans, and cilantro
Toss the shrimp with 2 tablespoons olive oil and salt. Meanwhile, heat a large sauté pan over a medium flame....
- by Dr. Aviv
- Tuesday July 28, 2015

